
23 Nov Pandemic mitigation for everyone: Ethnic differences in Wales
It is often repeated that in this pandemic storm we have to face the same rough sea but are on different boats. If this is true, it means that people also experience the pandemic and government-instated regulations differently. This is certainly the case for people from Black Asian and minority ethnic (BAME) background as compared to white people. But in what ways do these differences manifest? This blog post explores how the pandemic and mitigation services are considered differently by BAME and white people and how this translates into by both groups. What follows are the results of a survey study that ran from late January until mid-March 2021in the Swansea and Neath Port Talbot area in South Wales.
The Survey
The survey was commissioned, designed, and set up by the ‘Swansea Bay Regional Test Trace Protect Communications Cell’, which consists of two local councils and affiliated services, and secondary, further, and higher education institutions, BAME organisations, and a local police force. It gathered the input of 1112 respondents, of which 800 identified as White (British and Welsh) and 155 as BAME (including mixed-race). The remainder included White (other) or was left blank. The full report on which this blog post is based can be downloaded here.
Wales in the COVID-19 pandemic
Compared to other countries, in all waves. From the 26th of March 2020 onward, the four nations (Northern Ireland, Scotland, England, and Wales) have followed their own pandemic policies. These policies have been largely similar in nature, for instance in terms of restrictions on international travel, but differed in strictness and duration. For instance, At the time of writing in November 2021, Wales still requires mask-wearing in most public indoor spaces, unlike England. Compliance with the rules is considered to be good compared with other UK nations, and vaccination levels are amongst the highest in the world. However, still many lives have been lost, and there are strong inequalities between different ethnic groups in mortality rates. Indeed, people with a BAME background have been disproportionately affected by the COVID-19 pandemic in comparison to white populations (Public Health England, 2020; First Minister’s BAME Covid-19 Advisory Group, 2020). As such, this group has been marked as vulnerable by public health officials.
Estimations of being vulnerable
To be vulnerable is to be open to being affected – through our bodies and psyche. By virtue of being mortal and living in human bodies, everyone is vulnerable to suffering and death. However, changing contexts mark how at different times, in different places, and in different circumstances we are more or less vulnerable in different ways (cf. Cole, 2016). The manner in which people consider themselves vulnerable may impact their decision to get tested when they have symptoms and whether they comply with the requirements of the contact tracing programme. By extension, tA person’s orientation towards their own vulnerability may also reflect how they think about that of others and behave accordingly. In turn, this suggests if and how they comply with behavioural pandemic guidelines, for example how strongly they adjust their behaviour to ensure that they keep a safety distance of two meters to others or wear their masks in public indoor spaces.
In terms of estimations of personal vulnerability, ethnic differences are pronounced relatively strongly in the survey (see Figure 1). Some ethnic groups (e.g. ‘Indian’ and ‘White: Other’) considered themselves decidedly less vulnerable than the combined groups of Black and mixed Black people. In overall terms, the clinical indication that BAME people would be more vulnerable to illness and death due to a COVID-19 infection than white people (Public Health England, 2020) does not reflect in the BAME respondent’s estimations of their own vulnerability The survey does not provide definitive answers as to why that might be the case. However, under neoliberalism, vulnerability is associated with weakness and dependence (Cole, 2016); thus, accepting being vulnerable also requires accepting these other negative traits.
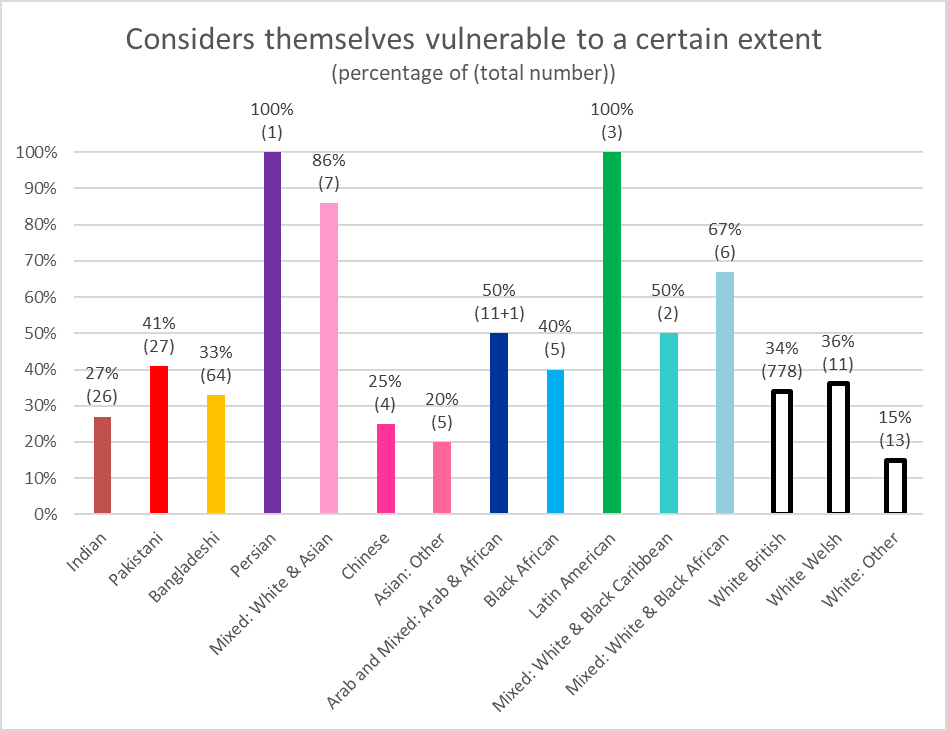 Figure 1: Vulnerability division along ethnicity lines
Figure 1: Vulnerability division along ethnicity lines
Getting tested
In terms of people’s willingness to get tested for COVID-19, few differences persist between the groups, except for age difference: higher proportions of younger white people and older BAME people have reported having been tested (see Figure 2). This could be explained by the higher likelihood that older BAME people live in the community with their family for longer than their white counterparts and that they might feel more exposed to the virus, which would merit testing. As older white people are less likely to live with extended family than their BAME counterparts, it would reduce their need to get tested.
The high number of young white people (aged 16-24) who had done a COVID-19 test could be explained by having been in more situations that would make them feel more exposed to the virus, such as (mass) social events, co-habiting, and working in people-facing jobs. The likelihood of having been in a situation in which they would potentially be infected is compounded by students going through the early lockdowns in shared accommodation. University students tend to be overrepresented by white people, which may contribute to the difference in the testing rates among white and BAME 16–24-year-olds.
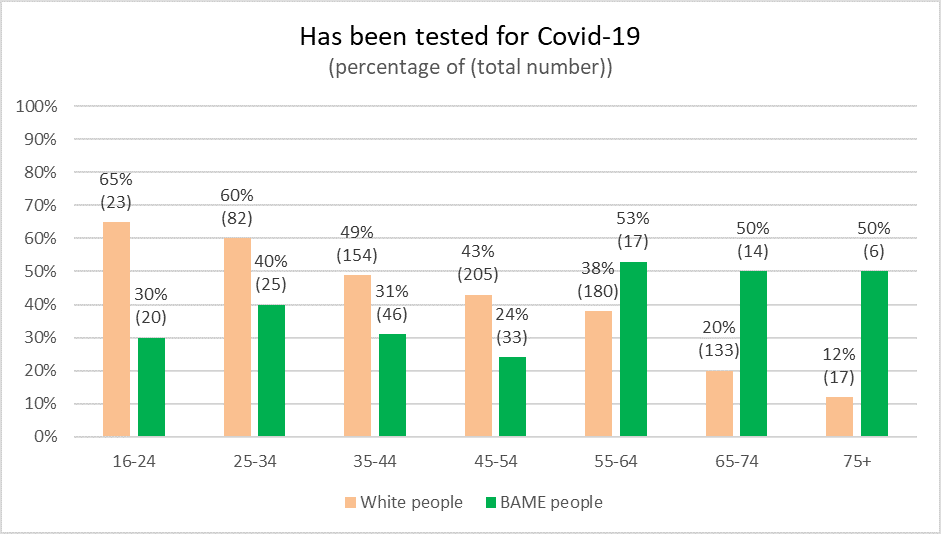
Figure 2: Divisions of usage of Covid-19 testing facilities along age lines
Vaccine uptake
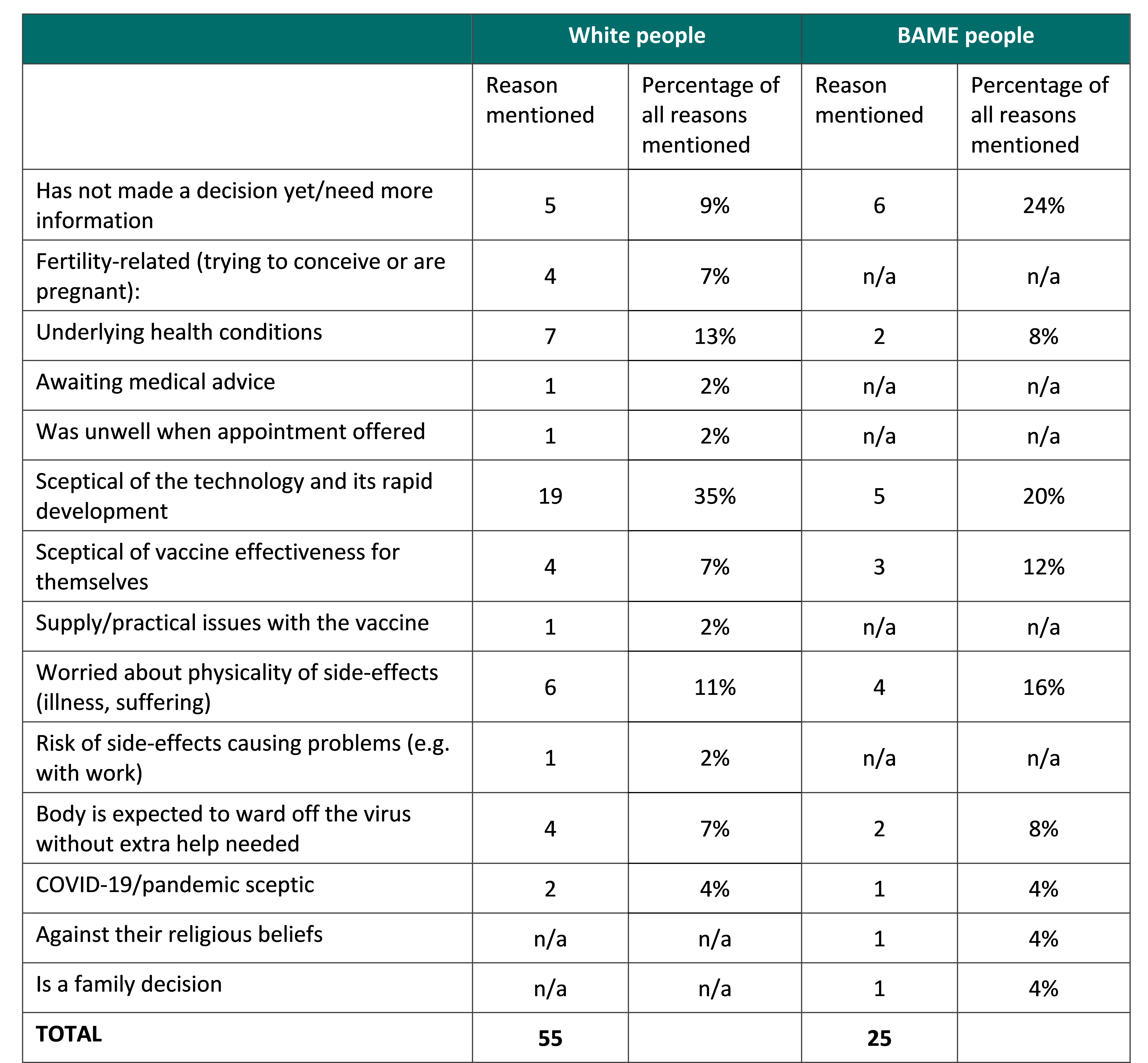
Remarkable differences pop up when it comes to the intention and acceptance of the invitation to get vaccinated. 91% of the white respondents said ‘yes’ to being asked if they would be vaccinated when invited, with 7% remaining unsure. Only 75% of the BAME respondents confirmed that they want to be vaccinated and 20% disclosed being uncertain about vaccination. One reason for this hesitancy was scepticism around the quick development of the vaccine and its effectiveness, and that participants needed more information to make their decision (see Table 1). For white people, the concerns seem to centre slightly more around biomedicine; as pivotal in the technology and in one’s personal medical circumstances. This is less pronounced in the answers of BAME people. Their answers seem to point out that social, cultural, and spiritual aspects of life play a larger role in the decision to get vaccinated. This finding is corroborated by Reid and Mabhala (2021) who explore the possible reasons behind it in more depth.
The survey does not fully capture the more complex, nuanced, and not always tangible experiences of BAME people who are medicalised and receive care or treatment. However, the percentages and reasons listed in Table 1 do reflect a wariness of and deeper concern for the medical and clinical care provision in Wales, and are in line with the results in similar surveys outside Wales (e.g., Freeman, 2020). Freeman (2020) and Morgan (2021) suggest that a reluctance to get vaccinated reflect the legacies of the violent histories of biomedicine vis-à-vis Black people through its eugenicist roots in the late 1800’s that systematically sought to physically, morally, and intellectually elevate white people at the expense of Black people. These painful histories also build on the experiments on Black people, such as the Tuskegee Syphilis Study, traces of which still seem to haunt modern-day biomedicine. For instance, the belief that Black people would have a higher pain threshold is still current in biomedical discourse (Hoffman et al., 2016) in addition to other discriminatory practices. Although such ethnicity-related experiences may not be profound and disruptive at the moment, their accumulation over a lifetime does erode trust and faith in the healthcare system and in the state. Whilst a lack of trust and faith in the healthcare system is beyond the COVID-19 vaccine and coronavirus pandemic, these are contextualised by these race-related anxieties.
Table 1: Reasons for refusing or doubting to take the offer of a vaccine in the past or future
The need for an ethnically sensitive approach
To lower discrepancies in terms of suffering the harmful effects of the pandemic between white and BAME people, the mitigation measures, as well as the communication of these measures, need to take ethnic differences within populations into account (Burgess et al., 2021; Razai et al., 2021). The generic idea that people will protect their biological body by utilising all available mitigation, such as the NHS tracing app and visiting test and vaccination centres, unless they do not have the capacity is not enough to understand the uptake and opinion of these services. Rather, the understanding of the existence and purposes of testing and vaccination needs to be placed in the context of people’s everyday realities. Future responses to COVID could therefore be more successful in reducing disproportionate suffering along ethnic lines if pandemic policies, policy operationalisation, and communication have a particular sensitivity to the racial contexts of living in South Wales and earlier encounters with medical services. Reid and Mabhala (2021) flag up that in some places in the UK faith-based organisations and ethnic group communities now play an active role in the communications around vaccination programmes that do not only involve, but are guided by BAME people, and more fully address deep-rooted historical concerns could help reduce the disproportionate suffering by BAME people compared to white people in this pandemic.
Authors: Diana Beljaars, Sergei Shubin (Department of Geography, Swansea University), and Louise Condon (Department of Nursing, Swansea University)
References
Burgess, R.A., Osborne, R.H., Yongabi, K.A., et al. (2021). The COVID-19 vaccines rush: participatory community engagement matters more than ever. Lancet, 397: 8-10.
Cole, A. (2016). All of Us Are Vulnerable, But Some Are More Vulnerable than Others: The Political Ambiguity of Vulnerability Studies, an Ambivalent Critique, Critical Horizons, 17:2, 260-277, DOI: 10.1080/14409917.2016.1153896
First Minister’s BAME Covid-19 Advisory Group (2020). Report of the Socio-Economic Subgroup. Accessed 4-10-2021.
Freeman, D. (2020). COVID-19 vaccine hesitancy in the UK. Accessed on 6-10-2021.
Hoffman, K. M., Trawalter, S., Axt, J. R., & Oliver, M. N. (2016). Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proceedings of the National Academy of Sciences of the United States of America, 113(16), 4296–4301.
Morgan, W. (2021). Poor vaccine take-up in BAME communities is not just down to hesitancy. The Conversation, March 1, 2021, Accessed on 6-10-2021
Public Health England (2020). Disparities in the risk and outcomes of Covid-19. Accessed 4-10-2021.
Razai, M.S., Osama, T., McKechnie, D.G.J. and Majeed, A. (2021). Covid-19 vaccine hesitancy among ethnic minority groups. BMJ, 372: n513.
Reid, J.A. and Mabhala, M.A. (2021). Ethnic and minority group differences in engagement with COVID-19 vaccination programmes – at Pandemic Pace; when vaccine confidence in mass rollout meets local vaccine hesitancy. Israel Journal of Health Policy Research 10, 33.
